
Horner’s Syndrome
Horner’s syndrome is a condition caused by damage to the nerve pathway that leads from the brain to the eye and face on the affected side of the body. It is considered a rare condition, affecting only 1.42 out every 100,000 people under the age of 19. Around one in every 6,250 cases of Horner’s syndrome happen at birth, and 65 percent of the cases are from birth injuries or trauma.
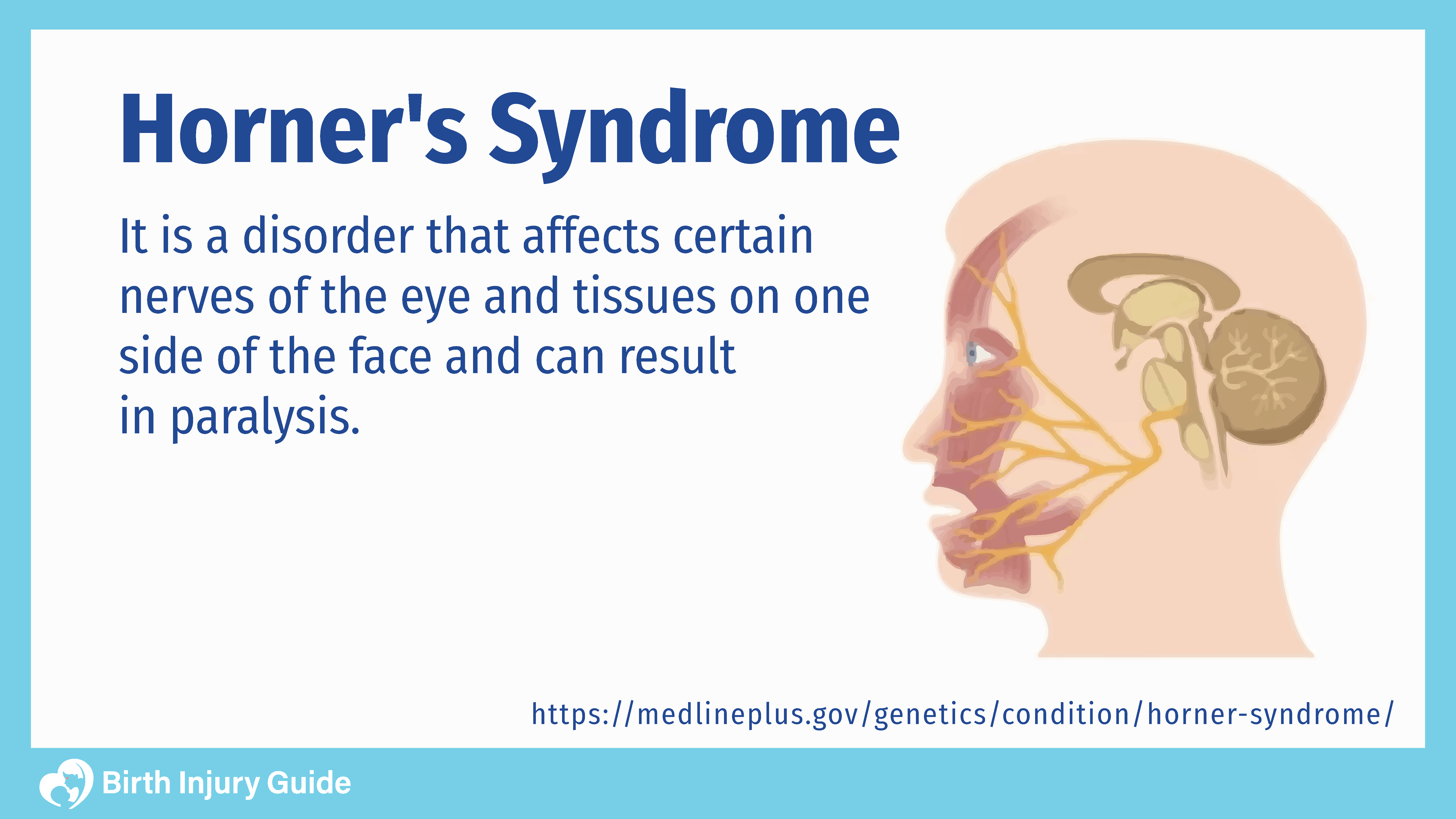
What is Horner’s Syndrome?
Horner’s syndrome occurs when there is a disruption in the nerve pathways from the brain to the face and eye. This condition generally only affects one side of the body and is marked by a decrease in pupil size, droopy eyelid and decreased sweating on the affected side of the face.
What Causes Horner’s Syndrome?
There are a variety of causes to Horner’s syndrome, but infants typically develop the disorder either congenitally or via an injury during childbirth.
Congenital Causes:
- Artery problems
- Carotid artery ischemia
- Lack of proper development of the carotid artery
- Genetic
- Unknown reasons
Birth Trauma Causes:
- Improper use of forceps during delivery
- Failure to properly detect abnormal fetal position (breech, etc.) and deliver in time
- Pulling too hard on the infant, causing tears to the sympathetic nerves
- Newborn shoulder dystocia and damage to the brachial plexus-nerves that supply the neck and arms
- Failure to respond to fetal distress in time
- Failure to schedule and perform a cesarean section (C-section) surgery in time
Can Horner’s Syndrome be Prevented?
Because Horner’s syndrome is often the result of other injuries, the best way to prevent the condition is to ensure adequate care during pregnancy, labor and delivery. Talk to your doctor about any risk factors you have that could lead to complications or birth injuries.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.
Horner’s Syndrome Symptoms
Horner’s syndrome symptoms are typically limited to the side of the affected face. Some infants may experience every symptom while others may have only one or two. The most common symptoms include:
- Miosis in the affected eye (constricted pupil)
- Different pupil sizes
- A delayed time in dilation when the affected pupil is under a dimmed light
- Ptosis: drooping of the affected upper eyelid
- The affected eye may appear sunken
- Little to no sweating on the affected side of the face
- The affected eye may appear bloodshot
- Lack or redness or a “flushed face” appearance after extreme heat or physical activity
- The iris in each eye may be a different color
Tests to Confirm Diagnosis
When an infant shows symptoms of Horner’s syndrome, a pupil dilation test is usually administered to see how the pupil responds to stimulation. A physical exam may follow, accompanied by an MRI to determine any birth injuries that may have led to the disorder. In some cases, a urine catecholamine test may be ordered.
Treatment
There is no specific treatment for this condition, but physicians typically identify and treat the underlying reason that the disorder developed. For instance, if it was caused by a brachial plexus injury, the nerves in the brachial plexus must heal in order to treat Horner’s syndrome. In some instances, the nerve injuries will clear up naturally, but in other cases, medication and/or surgery may be required.
Prognosis
While Horner’s syndrome may clear on its own or heal with medication and surgery in some infants, others may experience lifelong problems with the affected side of the face. The prognosis will greatly depend upon the severity of the disorder as well as how quickly it’s detected and treated. For example, if an infant suffers from oxygen loss after a difficult birth, Horner’s syndrome may clear eventually, but the baby may develop cerebral palsy or other serious disorders as a result of oxygen loss. Furthermore, if the treatment for the underlying problem is not successful, an infant may live with long-term injuries to the affected side of the face.
How to Optimize Your Child’s Prognosis
Generally, the prognosis for Horner’s syndrome is favorable. Of course, we have noted that the key to treating this condition is treating the underlying cause. To that end, the best way that you, as a parent, can optimize your child’s prognosis is to work closely with his or her healthcare team. Work together to determine the exact cause of your child’s injuries and find treatment options that will benefit his or her overall health.



