
Was your newborn diagnosed with hypoxic ischemic encephalopathy?
Was your newborn diagnosed with hypoxic ischemic encephalopathy?
"It was such a good feeling… thinking there are some people who are concerned about my problem."
Shahpoor S. Client Testimonial
Hypoxic Ischemic Encephalopathy (HIE) is a type of neonatal encephalopathy. When neonatal encephalopathy is indisputably due to hypoxic ischemic brain injury (anoxic: lack of oxygen), it is referred to as neonatal hypoxic ischemic encephalopathy. That is to say, this type of brain damage occurs when there is a lack of adequate oxygenated blood flow to the brain, a lack of adequate inspired oxygen or inadequate oxygen-carrying capacity in the blood.
Neonatal encephalopathy can be caused by many things including impaired maternal oxygenation, inadequate blood flow in the placenta, umbilical cord issues such as true knot formation, placental abruption, uterine rupture, umbilical cord prolapse and fetal issues like hemorrhage or thrombosis. HIE is preventable through careful monitoring during the prenatal period and during labor and delivery. Furthermore, the damaging effects of this disease, including brain damage, can be mitigated through timely recognition and intervention.
How Serious is it?
Hypoxic ischemic encephalopathy is a dangerous condition that requires immediate medical intervention. According to the National Institutes of Health (NIH), it affects approximately 1.5-2.5 out of every 1,000 full-term births in developed countries. Most importantly, the incidence rate in babies who are severely premature (born at 32 weeks gestation or earlier) is up to 60% of all live births. HIE can affect term infants, but it is much less common.
For babies that develop hie, the seriousness of their condition and the likelihood of complications depends on numerous factors relating to their health, other medical conditions and other birth injuries. Such factors include:
- Severity of oxygen deprivation: If oxygen deprivation was lengthy or entirely cut off, there is a greater chance of brain injury.
- How long the baby was deprived oxygen: The longer a baby goes without adequate oxygen, the more likely he or she will have permanent brain damage.
- The overall condition of the baby: Babies who are premature or who have other medical conditions are more fragile and vulnerable to brain injury from a lack of oxygen.
- How the baby’s care is managed: Recognizing and immediately treating oxygen deprivation is the key to preventing complications and permanent brain injury damage.
Terms
Hypoxic Ischemic Encephalopathy (HIE) or birth asphyxia are brain dysfunctions caused by a lack of oxygen or blood flow to the brain. This lack of perfusion causes damage to the brain and other organs. Hypoxia means not enough oxygen. Ischemia means not enough blood flow. Finally, the term encephalopathy refers to brain dysfunction. Therefore, hypoxic-ischemic encephalopathy is oxygen deprivation at birth that occurs close to labor and delivery that causes brain damage. If HIE develops after birth, you may also hear the term perinatal asphyxia, perinatal hypoxic ischemic encephalopathy or hypoxic ischemic brain injury.
You may also see the terms spelled differently, such as hypoxic ischaemic encephalopathy, neonatal hypoxic ischaemic encephalopathy or perinatal hypoxic ischaemic encephalopathy.
What Causes it?
There are a number of different possible causes and risk factors for hypoxic ischemic encephalopathy (HIE). Any of which can occur before, during or after the baby is born. For instance, various problems or medical complications may cause it during pregnancy in the antepartum period, or just before birth.
Antepartum causes:
Antepartum refers to the period just before childbirth. This includes the days and hours just before labor and delivery begin. Some causes that occur during this time include:
- Maternal diabetes with vascular disease
- Problems with blood circulation to the placenta
- Preeclampsia
- Chronic hypertension
- Cardiac disease
- Congenital infections of the fetus
- Drug and alcohol abuse
- Severe fetal anemia
- Lung malformations
Additionally, HIE can also occur and cause permanent brain damage during labor and delivery, or the intrapartum period.
Intrapartum causes:
The intrapartum period is the period during childbirth. This is the period when labor is active, and/or the process of delivery has begun. Causes during this time include:
- Excessive bleeding from the placenta.
- Maternal low blood pressure.
- Umbilical cord collapse or prolapse.
- Prolonged late stages of labor.
- Abnormal fetal presentation.
- Ruptured placenta or uterus.
In addition, infants can develop HIE due to complications that occur in the postpartum period, or after delivery. Furthermore, premature babies are particularly at risk of suffering brain injury or, even death if HIE occurs after delivery.
Risk factors for postpartum:
The postpartum period is the period of time just after a baby is born. This is the period just after birth, including the first hours or days that the infant is hospitalized. Risk factors during this period include:
- Severe cardiac or pulmonary disease.
- Serious Infections, including sepsis and meningitis.
- Severe prematurity.
- Low neonatal blood pressure.
- Brain or skull trauma.
- Cardiac arrest.
- Respiratory failure.
In some cases, there are no identifiable causes for infant hypoxic ischemic encephalopathy. It is important that healthcare providers and parents understand risk factors and symptoms and take action quickly if they suspect a newborn has HIE.
Symptoms
Sometimes, an infant that is still in the womb can exhibit signs of HIE or other hypoxic ischemic injury. Fetal distress is one of the most common signs of HIE or other oxygen-depriving event. During or after birth, the symptoms may vary depending on the child’s health and other factors. Some of the most common neonatal hypoxic ischemic encephalopathy (HIE) symptoms include:
- Low Apgar scores, <5 at 5 minutes and 10 minutes.
- Floppiness, or unreactive to sights or sounds, or more tense and agitated.
- Low heart rate.
- Low blood pressure.
- Poor muscle tone and absent reflexes.
- Weak breathing, no breathing at all, or rapid breathing.
- Need for resuscitation after delivery.
- Weak cry.
- Bluish or pale skin color.
- Excessive acid in the blood.
- Seizures or abnormal movements.
- Problems feeding.
How It Can Affect Children
The effects of Hypoxic ischemic encephalopathy (HIE) vary from patient to patient depending on whether the infant has mild HIE or moderate or severe hypoxic ischemic encephalopathy symptoms. Moreover, these symptoms will vary depending on the hypoxic-ischemic encephalopathy grade (mild, moderate, or severe). Infants with HIE may have minimal symptoms, which may not impact their lives in significant ways. On the other hand, children with more moderate or severe brain injury typically have more significant symptoms, such as those related to cerebral palsy. But, infants who suffer severe hypoxic ischemic encephalopathy at birth have a higher rate of brain damage and infant mortality (death) within hours of birth or the following days.
Some patients even require the assistance of a PEG tube for feeding; and a tracheostomy, with or without ventilator support for breathing assistance. So, many of the developmental issues associated with HIE are difficult to determine until the child is older. Often, developmental delays are not noticeable until the child misses developmental milestones, such as walking, talking, eating, and engaging in playtime.
Cerebral palsy is one of the most significant outcomes related to hypoxic ischemic encephalopathy and ischemic encephalopathy. Cerebral palsy affects as many as 10,000 infants and children each year. This group of motor disorders causes difficulties with movement, balance and coordination. In severe cases, children suffer from immobility or paralysis. If you suspect that your child has cerebral palsy, talk to your doctor to find out about options for managing symptoms and improving your child’s prognosis. There is no cure for cerebral palsy, but treatment options can improve your child’s quality of life.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.
Tests to Confirm a Diagnosis
Depending on the circumstances of your child’s birth, your health care team may do some tests immediately after birth to determine if the baby has suffered a hypoxic ischemic injury or is at risk for brain dysfunction. This most often happens in cases when labor is prolonged or difficult, there are umbilical cord problems or the baby has an obvious brain injury. Because immediate diagnosis and treatment are important for preserving the baby’s health, babies are often monitored for signs of hypoxic ischemic encephalopathy in the hours, days and weeks following birth. This is especially true for infants born prematurely or those with other medical conditions.
Infants born under traumatic circumstances or who are oxygen-deprived should be immediately assessed for hypoxic ischemic encephalopathy. As health care providers monitor newborns, they may order a series of tests or monitoring procedures. Follow your doctor’s medical advice for tests that may confirm your child’s diagnosis.
General assessments to determine if an infant has HIE include:
- Evaluation of respiratory status
- Need for respiratory support
- Cardiac status
- Neurological status
- Laboratory results
- Monitoring of urinary output
Labs tests include blood gasses, CBC (complete blood count), blood sugar, renal function studies, creatinine, electrolytes, and liver function studies like bilirubin, ALT (alanine transaminase), and AST (aspartate transaminase). Moreover, infectious disease labs like blood cultures and CRP (C-reactive protein) are often drawn.
Tests to further evaluate hypoxic ischemic encephalopathy include computerized tomography (CT scan), magnetic resonance imaging (MRI), echocardiography, and an ultrasound of the head. Other optional tests may include electrocardiogram (EKG), electroencephalogram (EEG), and evoked potential tests. Generally, patients with HIE are evaluated to determine the severity of the injury, which can be mild, moderate or severe. Infants with mild HIE usually have favorable prognosis’.
Treatment Options
How is hypoxic ischemic encephalopathy treated? Doctors have various alternatives for treating hypoxic ischemic encephalopathy (HIE). Certainly, these options depend on the cause of the condition and the amount of damage to the baby’s brain. Further, this makes it impossible for physicians to develop a definitive treatment for neonatal cases. Therefore, the primary goal of HIE treatment is to support the baby’s affected organs and prevent further brain injury.
Some of the most common options to treat it include:
- Mechanical ventilation to help a baby who can’t breathe without assistance.
- Cooling, or therapeutic neonatal hypothermia. Therapeutic hypothermia lowers the baby’s body temperature in order to reduce swelling and brain injuries. Also called whole body hypothermia, the American Academy of Pediatrics considers this one of the best treatment options to protect your baby’s brain.
- Hyperbaric oxygen treatment in cases where the cause of hypoxic ischemic encephalopathy HIE is carbon monoxide intoxication.
- Medications to control seizures.
- Treatments to assist the baby’s heart rate and function and control blood pressure.
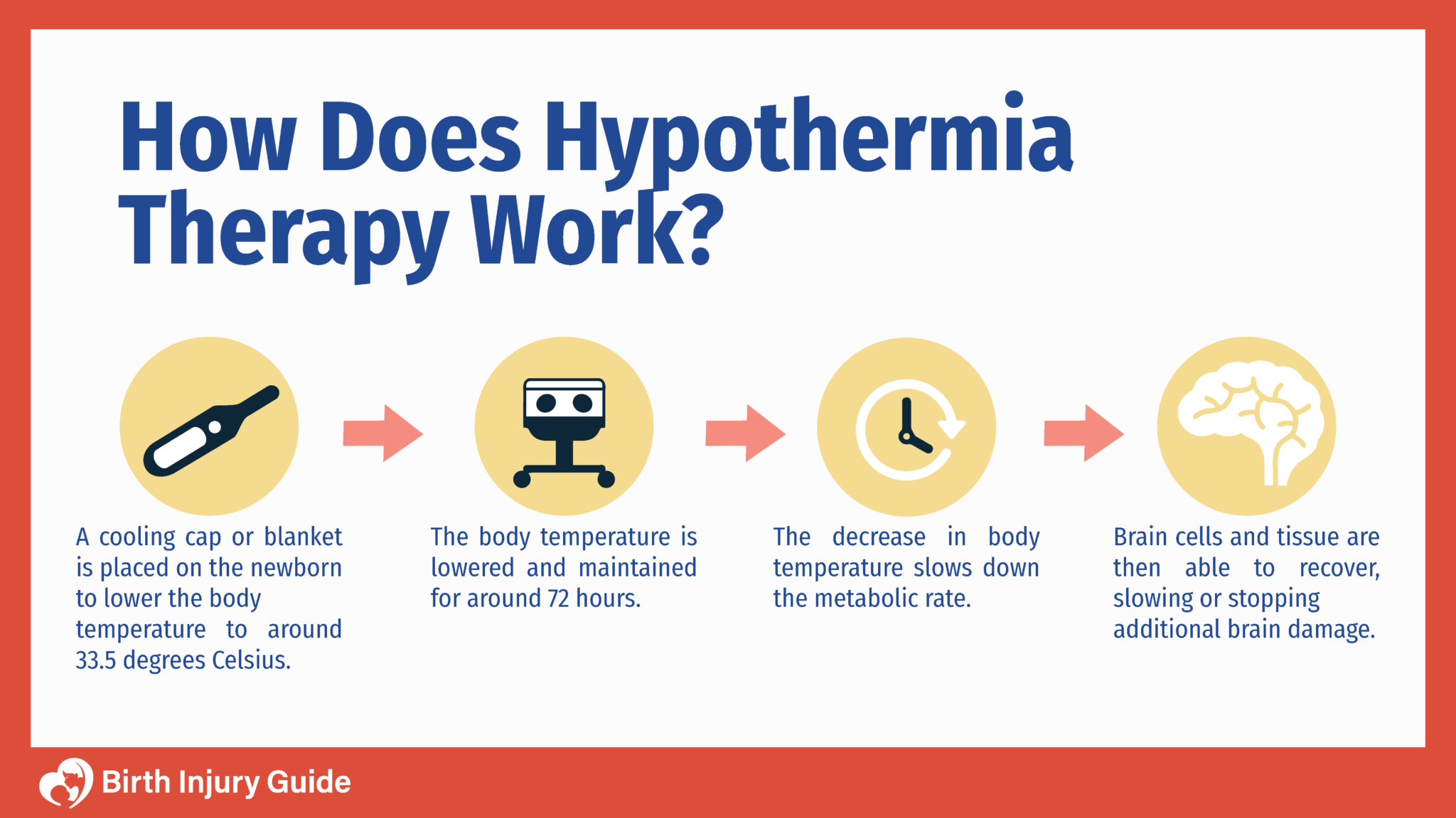
Therapeutic hypothermia treatment is one of the most common and successful means of preventing additional brain damage in infants with hypoxic ischemic encephalopathy. During therapeutic hypothermia, the infant’s body temperature is lowered to around 92 degrees (F). This temperature is maintained for 72 hours. The lowered temperature slows down the metabolic rate, which allows brain cells time to recover, and protects healthy cells from damage.
It is important that therapeutic hypothermia begins as soon as possible – preferably in the first six hours after the brain injury or HIE occurs. Failure to initiate treatment for HIE in a timely manner is a type of medical negligence.
If your child is diagnosed with hypoxic ischemic encephalopathy, he or she may be admitted to the neonatal intensive care unit, or NICU. NICU is a specialized intensive care unit in a hospital designed just for infants. There, doctors and nurses work round-the-clock to monitor infants and ensure they are getting proper warmth, nutrition, diaper changes and any necessary treatments or medications. Neonatal intensive care is highly specialized and you may meet with neonatologists and other specialists that you aren’t familiar with. These doctors and nurses have a tremendous responsibility to the infants in intensive care and their families.
Can HIE be Prevented?
There are some things that health care providers can do to prevent hypoxic ischemic encephalopathy, or at least reduce the risk of it occurring. The two primary things that healthcare providers can do are:
- Monitor: Closely monitor the health of the mother and the infant for signs of fetal or other distress.
- Take Action: If the mother or infant come under distress, the baby must be delivered as soon as possible.
During pregnancy, mothers can also help reduce the risk of hypoxic ischemic encephalopathy by attending all prenatal appointments and following their doctors’ advice. If the pregnancy is high-risk, then healthcare providers should take additional steps to ensure maternal and fetal health. In many cases, this includes referring the mother to a maternal-fetal specialist for additional prenatal care. Once labor has begun, heart monitors should be used to monitor the mothers and infants heart rate. Monitoring should continue throughout the labor and delivery process.
If at any time there are abnormalities or “nonreassuring heart tracings” on the monitors, healthcare providers should immediately take action. There are resuscitative measures that doctors can use to reduce the risk of brain injury due to oxygen deprivation. Such measures include increasing oxygen and blood flow, administering IV fluids to the mother or attempting to correct the abnormality by having the mother change positions. There is no guarantee that these measures will prevent hypoxic ischemic encephalopathy, but they are options available.
In cases where HIE is caused by obstetrical conditions, resuscitative measures are likely to be ineffective. Instead, healthcare providers should focus on delivering the baby as soon as possible and taking action immediately thereafter to protect the baby’s brain, diagnose and treat HIE or other birth injuries.
Prognosis
Determining the prognosis for a child with hypoxic ischemic encephalopathy depends on a variety of factors, including his or her overall health. Moreover, it can be difficult to predict long-term outcomes or complications. While estimating the prognosis for infants with HIE can be challenging, doctors have found certain criteria can help. Consider the following:
- A lack of spontaneous respiratory effort in the 20-30 minutes, without resuscitation, immediately after birth almost always leads to death.
- Seizures are a threatening sign. As a result, poor neurologic outcomes tend to be greater among infants who have seizures that are frequent or difficult to control.
- Abnormal clinical findings in the first 7-10 days of life often indicate a poor prognosis. Infants must be monitored carefully while in the neonatal intensive care unit, or NICU.
- Persistent difficulties related to feeding or abnormal muscle tone required to suck and swallow; may be a sign of damage to the central nervous system (CNS).
- Poor head growth during the postnatal period often is a predictor of neurologic deficits.
- An electroencephalogram (EEG) with normal background activity at around 7 days old is a positive prognostic sign.
Every child and birth injury are different. Talk to your child’s healthcare team about his or her prognosis. In conclusion, you should find out as much as possible about your child’s overall health and medical conditions. Babies that have hypoxic ischemic encephalopathy often develop complications that impact their lives long-term, such as:
- Cerebral Palsy: Some estimates suggest that around 30% of babies with moderate to severe HIE will develop cerebral palsy.
- Epilepsy: Around 16% of babies with moderate/severe HIE will develop epilepsy.
- Vision Issues: Around 14-17% of babies with moderate/severe HIE suffer from blindness.
- Hearing Issues: Six percent of babies with hypoxic ischemic encephalopathy suffer hearing impairments.
- Cognitive Impairment: Cognitive impairments may occur alongside disorders like cerebral palsy, or may develop on their own.
How to Optimize Your Child’s Prognosis
One of the best ways to optimize your child’s prognosis after an diagnosis of hypoxic ischemic encephalopathy is to be informed. Firstly, be aware of what HIE is and how it affects your child. In the flurry of activity that follows having a new baby and managing his or her care, all the terms and elements of hypoxic ischemic encephalopathy HIE can seem overwhelming. It is, nonetheless, important that you educate yourself as much as possible on what has happened to your child and how you can help him or her survive and thrive. Getting attention immediately after birth is critical for positive outcomes.
Secondly, be open-minded to treatment and therapy options that may help prevent further brain damage, such as cooling therapy. Treatments for hypoxic ischemic encephalopathy may seem somewhat unconventional, and your healthcare team can give you more information on what to expect. Give your child every opportunity to heal and recover. Remember that there is no cure for HIE, but treatments can help reduce the affects of damage and prevent further damage.
Finally, work with your child’s healthcare team to create a plan for his or her treatment in both the short- and long-terms. This is especially important if your child has cerebral palsy or other conditions that will affect them long-term. As your child gets older, the treatment options may change. If there are conditions like cerebral palsy or epilepsy, it will be important to routinely assess your child’s symptoms and progress and make changes to his or her care plan.
Tips for Living with a Birth Injury
Living with a birth injury like hypoxic ischemic encephalopathy is challenging for children and their families. For parents, optimizing your child’s prognosis is one of the most important focuses of your life. However, you also need to take time to remember to enjoy life as much as possible, and help your child do the same. Fortunately, there are some things that you can do to accomplish both of these goals – optimizing prognosis and improving your child’s quality of life. Our best tips include:
- Get Medical Advice: Talk to your healthcare team about things you can do to help your child at home, school, or at events.
- Be Active: If your child needs therapy, be active in those sessions, be it physical, occupational, behavioral, speech, or other therapies.
- Consider Counseling: If you have other children, you may find yourself juggling a lot of responsibilities and tasks that take time away from your family. Consider family counseling to help ensure that everyone in your family has their needs expressed and met.
- Set Goals: In your day-to-day life, help your child set goals that are realistic and attainable. Make a big deal out of it when goals are met, and be encouraging and constructive when goals are not met.
- Develop a Routine: Routine is important for children, especially those with special needs or disabilities. Setting a routine helps them understand what their responsibilities are and how the household functions on a daily basis. As parents, you may have to alter your routine somewhat to accommodate your child’s needs, but your household should function as “normally” as possible.
- Get Support: There are many local, state and national organizations that help support families affected by birth injuries and various medical conditions. If you are feeling lost or alone, it can be helpful to reach out for support from other families going through something similar. Organizations like the Cerebral Palsy Foundation and Hope for HIE offer valuable resources for families.
- Get Educational Support: When it is time to think about starting school, get support from your child’s school and teachers. Find out from his or her doctor if there are any accommodations needed, or if your child needs an individualized education plan (IEP). Then, work with the school to make sure your child is set up for success before ever stepping foot in the classroom.
Ultimately, helping your child live his or her best life takes a combination of your love and support, as well as that of healthcare providers, therapists, teachers, and others your child interacts with. The good news is that a diagnosis of hypoxic ischemic encephalopathy, cerebral palsy or another birth injury does not equal a poor prognosis or poor quality of life.



