
Placenta Previa
The placenta is one of the most important organs during pregnancy. It develops inside the uterus and is what provides oxygenated blood and nutrients to the baby. It also carries waste away from the baby. The placenta is connected to the umbilical cord, which is the baby’s lifeline. Placenta previa (pluh-SEN-tuh PREH-vee-uh) is a medical condition that occurs during pregnancy when the placenta covers the cervix. In some cases, the placenta only covers a portion of the cervix. In others, the placenta blocks the entire cervix. This can be dangerous as the pregnancy progresses, as the placenta will block the opening to the birth canal.
Women who have placenta previa may experience bleeding during pregnancy, and more heavy bleeding during delivery. Doctors recommend that women with this condition avoid anything that may cause contractions, including sexual intercourse, using tampons or participating in physical activities like jogging or running. If placenta previa does not resolve, you may require a cesarean delivery (c-section) rather than attempting vaginal delivery.
What is Placenta Previa?
Placenta previa is a potentially dangerous medical condition that occurs when the placenta develops lower in the uterus than is “normal”. There are three different types of placenta previa:
Marginal
Marginal previa occurs when the placenta is next to the cervical os or opening, but does not cover it.
Partial
Partial previa occurs when the placenta only covers part of the cervical os.
Complete
Complete previa occurs when the placenta covers the entire cervical os.
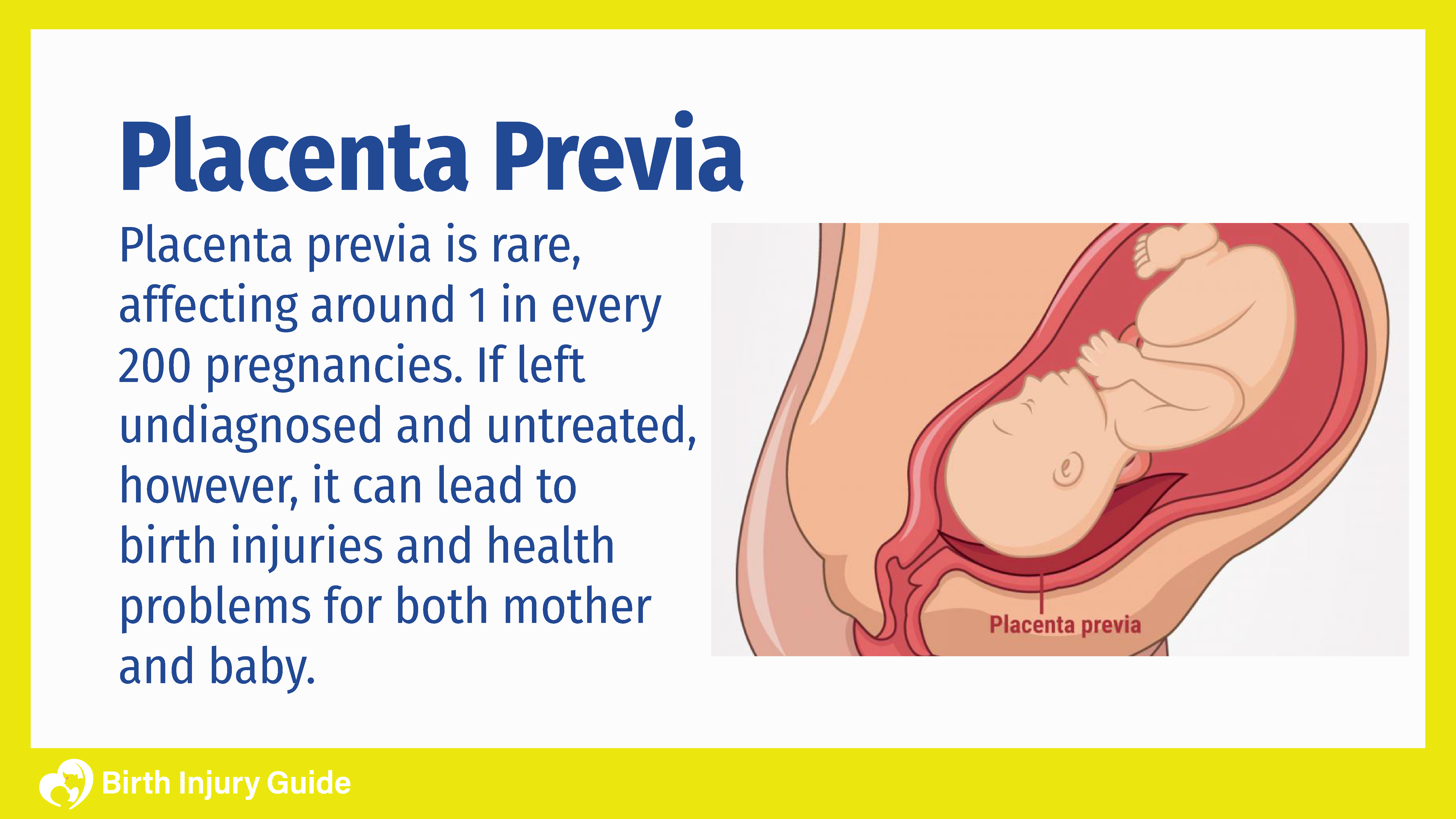
How Common is Placenta Previa?
Estimates suggest that around one in every 200 pregnancies suffers from some type of placenta previa. It is most common in women who have:
- Abnormally shaped uterus
- Numerous previous pregnancies
- Multiples (twins, triplets, etc.)
- Scarring on the lining of the uterus
- In vitro fertilization
Diagnosing and treating placenta previa is crucial to avoiding possible complications.
Health Risks of Placenta Previa
If placenta previa is diagnosed early in the pregnancy, it can be managed and generally doesn’t cause serious problems. However, as the pregnancy continues, if previa continues or worsens, there is the risk for potentially serious complications and health risks.
Infant Health Risks
Any type of placental issue can impact an infant, especially around the time of birth. Some of the possible health risks for baby’s include:
- Preterm birth
- Congenital abnormalities
- Respiratory Distress Syndrome
- Low birth weight
- Anemia
- Stillborn birth
Maternal Risks include
Mothers are also at risk for health problems when the placenta is in the wrong place or isn’t functioning properly. If the placenta is low in the uterus when labor begins, the process of the cervix opening and thinning out can cause the blood vessels that connect the placenta to the uterus to tear. This can cause severe bleeding, and can lead to:
- Hemorrhaging
- Hysterectomy
- Shock
- Death
Placenta Previa Causes
During pregnancy, a woman’s placenta moves as the uterus expands and stretches. During early pregnancy, the placenta typically lies low, and as the womb increases in size, it moves to the top portion. In fact, towards the end of the pregnancy, and by the third trimester, the placenta should be at the top of the womb, away from the cervix. Women with placenta previa, however, will experience a full, partial, or marginal cervix blockage due to the placenta staying towards the bottom of the womb.
In many cases, placental separation is due to uterine factors. For example, scarring of the tissue lining of the uterus can occur from previous cesarean section (C-section) deliveries, D&C procedures or abortions. This scarring heightens the risk of a woman having placenta previa.
Another cause of placenta previa involves placental issues. Carrying more than one baby, smoking cigarettes and living in an area with a higher altitude can cause the placenta to grow larger than normal in order to compensate. As a result, a larger placenta may not stretch far enough to be away from the cervix.
Medical Negligence
Some injuries caused by placenta previa may actually be due to medical negligence. When doctors fail to properly diagnose and treat this condition, both mom and baby are at risk for health problems. Some of the ways that medical negligence may occur include:
- Failure to monitor an infant after a diagnosis of placenta previa, which can lead to fetal hypoxia.
- Failure to conduct ultrasounds and formulate a correct plan of action.
- Attempting a normal delivery when complete placenta previa is present.
- Delaying or not scheduling a C-section.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.
Risk Factors
In addition to what causes placenta previa, there are some risk factors that may contribute to it, or increase the risk. These include:
- Maternal age of 35 and older
- Prior pregnancies with the condition
- Prior births
- Scar tissue from abdominal surgeries
- Maternal diabetes
- History of smoking or cocaine use
- Are Black or Hispanic
Placenta Previa Symptoms
The primary symptom associated with placenta previa is a sudden onset of vaginal bleeding, which may or may be accompanied by cramps. Vaginal bleeding will vary in severity according to each person. Bleeding often occurs at the end of the second trimester or at the beginning of the third.
If placenta previa is diagnosed early in the pregnancy, there is a chance that it will resolve without treatment. As the pregnancy progresses, doctors will monitor the position of the placenta and assess any other symptoms that develop.
Women should be aware that a sudden onset of bleeding during pregnancy could be a medical emergency. Bleeding from placenta previa can be serious enough to be life-threatening. It is important to contact your doctor immediately if you start bleeding while pregnant. Severe bleeding should always be treated as a medical emergency.
Diagnosing Placenta Previa
Doctors can diagnose placenta previa via an ultrasound. Sometimes a diagnosis can be made during a routine prenatal appointment where an abdominal or transvaginal ultrasound are performed. In other cases, doctors will order these tests after the mother reports vaginal bleeding. If the doctor suspects placenta previa, they will be careful to avoid any vaginal exams or tests that may disrupt the placenta or cause additional bleeding. They will also continue to monitor yours and the baby’s health to see if the placenta moves into the correct position as the pregnancy progresses. Doctors may initiate treatment if persistent placenta previa is a concern.
Placenta Previa Treatment Options
There is no cure for placenta previa. However, there are treatment options that can help promote a favorable outcome. Treatment options will greatly depend on the gestational age and the overall health of the infant. Also, it will depend on how severe bleeding is and/or if it has stopped, and the position of both placenta and baby.
For complete placenta previa, a C-section delivery is almost always the only option. C-sections are typically scheduled after 36 weeks gestation, but may be sooner if the bleeding is extreme and doctors can’t stop it.
For marginal and partial placenta previa, normal delivery may still be an option, but will depend on the extent of bleeding. For partial placenta previa, how much of the cervix is blocked will also be a factor in whether vaginal delivery is possible. Reducing activities and extended bed rest are almost always recommended in these cases.
Other treatment options may include:
- Blood transfusions
- Medications that help sustain a pregnancy until 36 weeks gestation
- Steroid shots to help the baby’s lungs mature
- Rhogam shots for Rh negative blood types
Prognosis
The most serious risk associated with placenta previa is severe, uncontrollable bleeding. When this occurs, infants may need to be delivered before their vital organs have developed, putting them at risk for a myriad of life-threatening health issues. Preterm birth has definite health risks. The good news is that neonatal intensive care units (NICUs) and healthcare providers that specialize in treating neonates are capable of doing great things to improve the baby’s prognosis. For parents, the idea of having a premature baby is scary, but in cases like those with placental issues, the rewards often outweigh the risks.
Physicians should always monitor pregnant women closely, especially those who have risk factors associated with placenta previa. Early detection and diagnosis may help the bleeding from getting too severe. In cases where the mother delivers and doctors can control or stop the bleeding, the prognosis is generally favorable. Unfortunately, some cases of placenta previa are so severe that the bleeding causes longer term complications for the mother. In the most severe cases, it can be fatal.



