Placental Insufficiency
The placenta is an organ that develops during pregnancy and is a lifeline for the baby. The placenta is what attaches to the umbilical cord and provides vital nutrients to the developing fetus. When the placenta does not function as it should or is damaged, it is called placental insufficiency. It may also be referred to as placental dysfunction, fetoplacental insufficiency, uteroplacental vascular insufficiency or uteroplacental insufficiency.
Placental insufficiency is a rare pregnancy complication affecting only one in every 300 pregnancies. However, it’s a serious complication. If not detected and treated immediately it can lead to life-threatening health complications for both mother and baby. When chronic placental insufficiency occurs, it can lead to fetal growth restriction, oxygen deprivation and other potentially dangerous medical conditions.
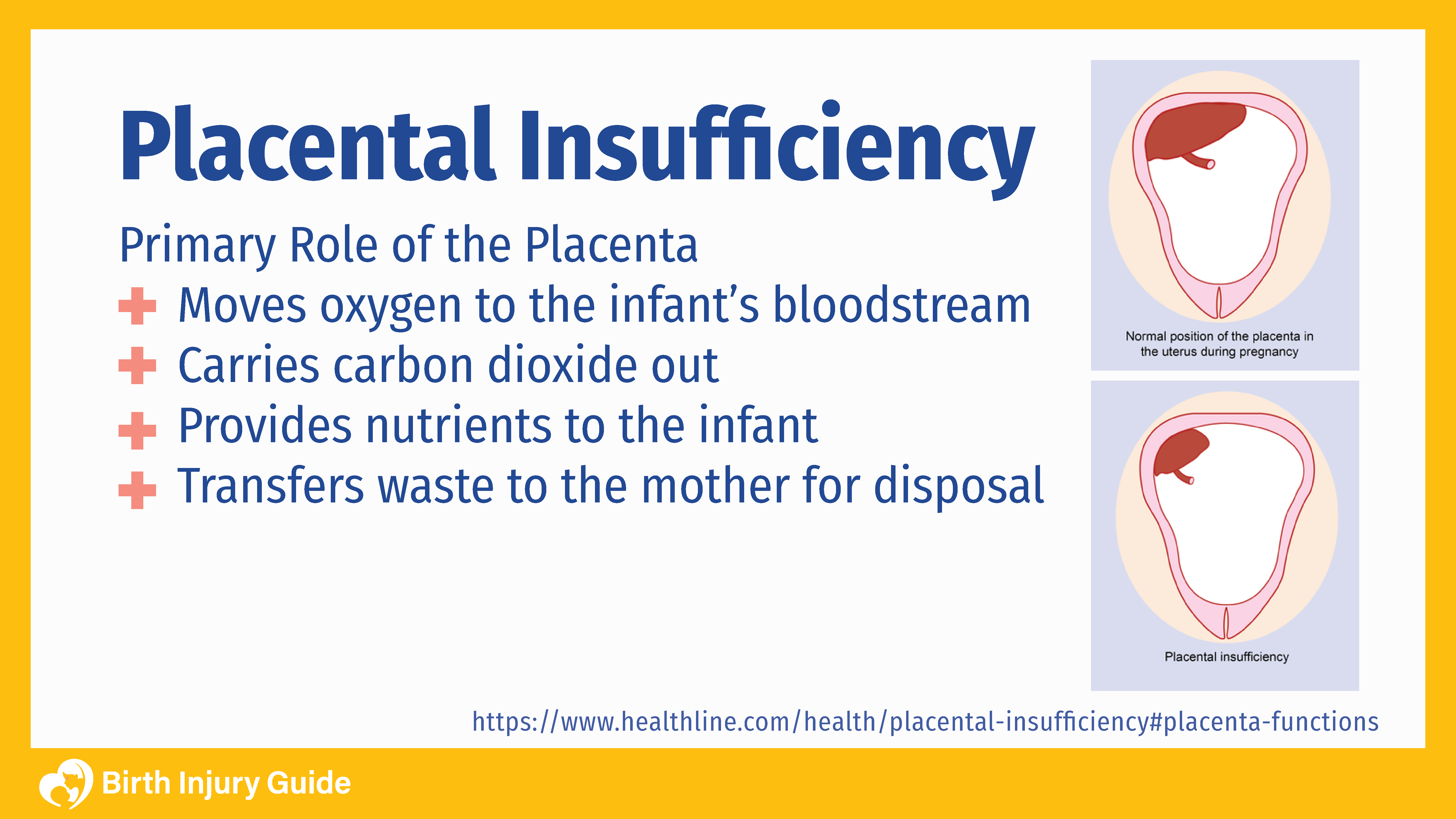
The Important Role of the Placenta
The placenta is a unique and complex organ. It forms and grows following conception. This process begins when the fertilized egg attaches to the wall of the uterus, and continues throughout the pregnancy. For a developing fetus, the placenta is an incredibly important organ. The umbilical cord connects the baby to the placenta and provides blood flow, oxygen and nutrients from the mother to the baby. The placenta is a filtration system and nutrient exchange system. During pregnancy, blood and oxygen from the mother collect in the placenta. The placenta filters out waste and then sends oxygen and blood to the baby.
What the Placenta Does
- Infusing oxygen into the baby’s bloodstream
- Removing carbon dioxide from the baby
- Delivering nutrients to the baby
- Eliminating waste from the baby
The placenta is also responsible for producing certain hormones during pregnancy and it protects the baby from infection. Over the course of the pregnancy, the placenta grows, reaching around 1-2 pounds by the time the baby is full-term.
What Causes Placental Insufficiency?
Placental insufficiency is a blood disorder marked by inadequate blood flow to the placenta during pregnancy. If blood flow is restricted, the infant is unable to receive adequate nutrients and oxygen, making it difficult for the baby to grow and thrive while in the womb. The earlier this condition surfaces in pregnancy, the more serious the health risks become.
The most common causes and risk factors include:
- Preeclampsia
- Gestational diabetes
- Anemia
- Smoking and/or taking illegal drugs
- Maternal blood thinner medications
- Maternal blood clotting
- Maternal cardiovascular disease
In addition to these risk factors, there are also a few emergent complications that can lead to placental insufficiency. For example, if the placenta is not adequately attached to the uterine wall, or becomes detached (placental abruption), it can result in placental insufficiency.
Placental Insufficiency Symptoms
Unfortunately, placental insufficiency doesn’t have any outward symptoms. However, women who have been pregnant before may notice less fetal movement when compared to previous pregnancies. They may also note a reduction in the baby’s movement. Mothers may also notice that their stomach does not seem to be growing as much as previous pregnancies. In most cases, the first signs of placental insufficiency are inadequate growth noted on ultrasound (intrauterine growth restriction), or signs of fetal distress or maternal illness. Mothers should report any changes in fetal behavior as soon as possible.
Diagnosis and Treatment
Adequate prenatal care by a qualified physician is imperative for the diagnosis and treatment of placental insufficiency. During prenatal appointments, doctors will do certain tests and examinations to determine how the pregnancy is progressing. During a routine ultrasound, problems with the placenta can be detected – in this case, a smaller uterus, a small placenta and the placement of the placenta. An ultrasound can also provide information about the baby’s size and weight. Additionally, checking the mother’s alpha-fetoprotein levels can help detect the condition, as well as monitoring and measuring the baby’s heart rate. These measures are more frequent during complicated pregnancies.
Since preeclampsia is one of the leading risk factors of placental insufficiency, getting the mother’s high blood pressure under control can help the infant thrive and grow. If the mother has gestational diabetes, blood sugar must be monitored and kept under control. Since preterm labor is a risk factor, some physicians may opt to give the mother steroid shots in order to strengthen the baby’s lungs.
There is no effective way to “fix” placental insufficiency. Instead, the goal of treatment is to carefully manage the situation and minimize the risk of possible complications or negative health outcomes. How the condition is treated will largely depend on the stage of pregnancy at the time of diagnosis as well as the stage of fetal development. Some of the possible treatment options include:
- C-section: Women in the later stages of pregnancy (35 weeks or later) may be treated via a scheduled c-section.
- Bed rest: If placental insufficiency is diagnosed in the earlier stages of pregnancy, the mother may be ordered to bed rest. This is common in a high risk pregnancy and can help reduce stress on the body and the baby.
- Monitoring for preeclampsia: Preeclampsia is a dangerous medical condition, and is one of the leading causes of placental insufficiency. It is important that women are carefully monitored for preeclampsia.
- Referral: Women who have placental issues may be referred to a high-risk fetal specialist.
- Steroids: Steroids do not treat placental insufficiency, but they can be useful in helping the baby’s lungs develop quicker. This is important if doctors believe that a c-section or preterm birth will be necessary.
Risks to Mother and Baby
In most cases, mothers are not at risk of death if placental insufficiency develops. However, preeclampsia, one of the most common risk factors of the condition, may heighten the risk. Preeclampsia alone brings on its own set of dangers to the mother, including extremely high blood pressure, abnormal weight gain, edema, protein in the urine and severe headaches. If preeclampsia develops into eclampsia or HELLP syndrome, the mother is also at risk for stroke, seizures, coma or death.
Risks to the Mother:
- Heightened risk of preterm labor and birth
- Placental abruption
- Ruptured placenta
- Bleeding and premature contractions
- Heightened risk of an emergency Cesarean surgery (C-section)
- Maternal infections
- Blood clotting
- Post-term pregnancy
Risks to the Baby:
For babies, the risks of placental insufficiency can be life-threatening, especially if it develops during the first trimester. Lack of adequate blood flow, oxygen and nutrients can lead to risks including:
- Oxygen deprivation at birth
- Brain damage
- Hypothermia
- Low blood sugar
- Intrauterine growth restriction (IUGR)
- Low birth weight
- Excessive red blood cell count
- Hypocalcemia (low blood calcium levels)
- Learning disabilities
- Stillbirth
Infants are also at risk for numerous birth defects. According to a study performed by the American College of Obstetrics & Gynecology (ACOG), an early onset of placental insufficiency places infants at a 40% higher risk of developing the following birth defects:
- Brain damage
- Lung dysfunction
- Gastrointestinal problems
Placental Insufficiency Prognosis
Although there is no cure for placental insufficiency, it can be managed with the correct medical diagnosis and intervention. The best outcomes for placental insufficiency occur when the condition is diagnosed between 12 and 20 weeks gestation. Early diagnosis and treatment are vital for not only the management of the condition, but also for the health of both mother and baby. It is critical that the mother attend all prenatal appointments and follow doctor recommendations.
The Risks of Brain Damage
Placental dysfunction, including placental abruption or insufficiency is a common cause of oxygen deprivation in infants. A partial or complete lack of oxygen for even a short amount of time can have devastating consequences. If a baby does not have adequate oxygen and nutrients while in the womb, the baby’s growth may be stunted, and they can develop brain damage. Brain damage can result in serious, life-long medical disorders including:
- Cerebral palsy
- Attention deficit hyperactivity disorder (ADHD)
- Autism
- Learning disabilities
Any of these conditions can have a profound impact on the baby’s prognosis. Conditions like cerebral palsy require extensive medical care and supervision, often lasting throughout the child’s life. Again, early diagnosis and intervention is the key to a positive prognosis.



