
Caput Succedaneum
Caput succedaneum is a medical term describing swelling that occurs to a baby’s scalp shortly after delivery. This birth injury is what causes the “conehead” shape of a newborn baby’s head. During childbirth, especially during head-first deliveries, pressure exerted on a baby’s head can damage the scalp. Fluid may then build up, which causes caput succedaneum, and may lead to other birth injuries as well.
Caput succedaneum is quite common, and generally is not a reason for alarm. Pressure and compression during vaginal birth is normal. Although it may cause slight discomfort for the baby, this is not a life-threatening birth injury in itself. It can, however, lead to additional health issues, such as jaundice. Jaundice is especially a risk if there is bruising to the infant’s head also. Infants are also at risk for alopecia (baldness) or infection in the area.
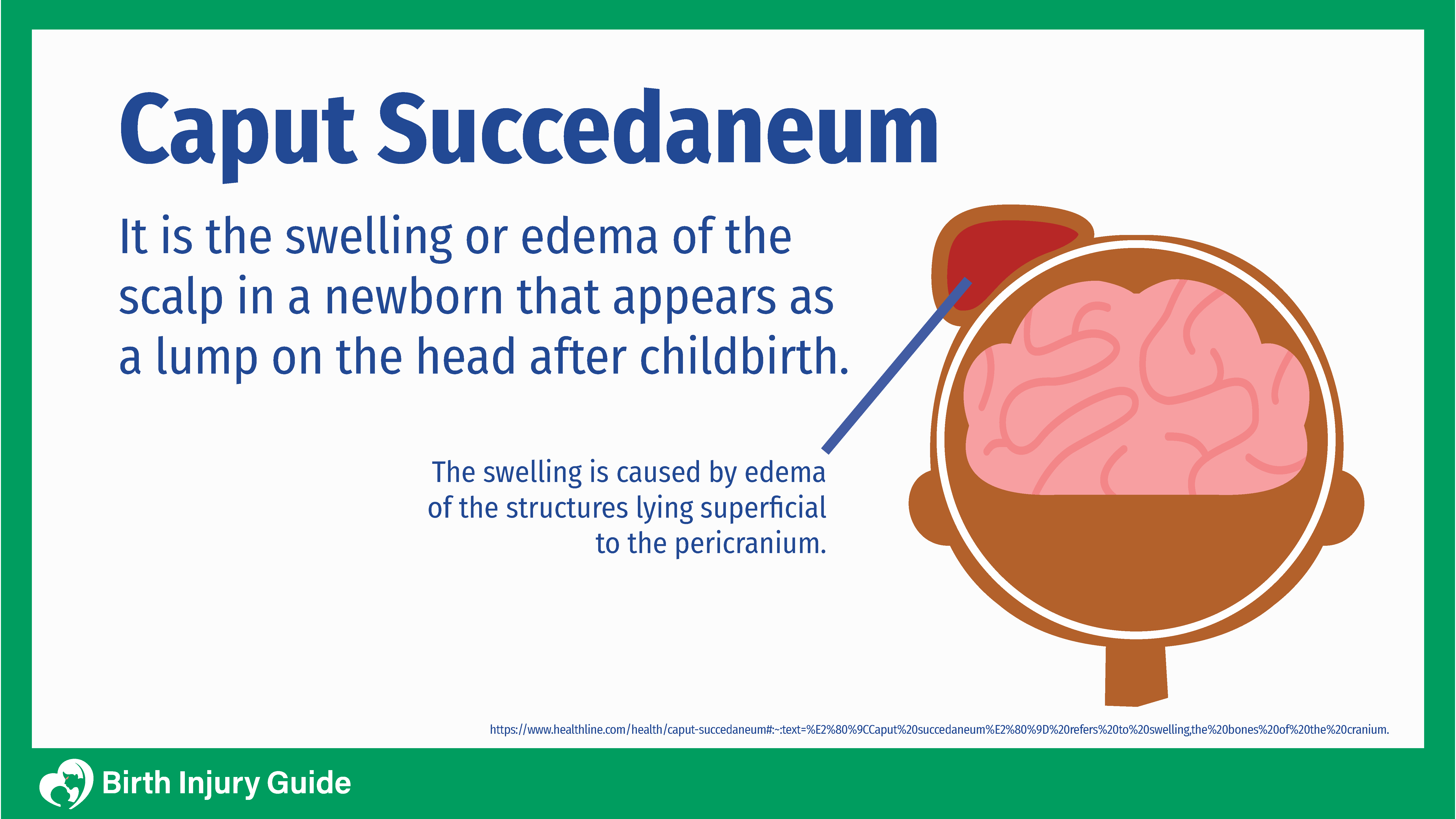
What is Caput Succedaneum?
Caput succedaneum is a type birth injury that causes swelling outside of the skull, but under the scalp and skin of a newborn baby. It often presents as a conehead shape, which can be disheartening for parents. This is different from the swelling that occurs when there is a hematoma on the baby’s head, such as with cephalohematoma. However, for new parents, it can be concerning to see what appears to be a deformity on their newborn baby’s head.
Caput succedaneum is a relatively common birth injury that occurs during vaginal birth. As the baby moves through the birth canal, there is pressure and compression around the body, including the infant’s head. This pressure can cause fluid buildup, bruising, and sometimes other injuries. This does not indicate a skull fracture.
The good news is that the swelling typically resolves within a few days unless there is bruising or additional complications. If bruising is present, the infant is at risk of developing jaundice, which can be dangerous if it is not properly diagnosed and treated. There is also a risk for hair loss (alopecia) in a ring shape around the skull.
What Causes Caput Succedaneum?
In most instances, caput succedaneum occurs after a long, difficult delivery. The pressure on the baby’s head usually occurs after the membranes break as the baby descends into the birth canal. It is most common when the baby is delivered head-first. That’s because the head-first delivery puts pressure in a localized area of the baby’s head as delivery progresses. The birth canal is a narrow passage and it takes some pressure to keep the baby moving toward delivery. Babies born via c-section can also have caput succedaneum, but this is most often due to pressure on the baby’s head before the c-section began.
Caput succedaneum can also occur during deliveries that involve:
Premature Rupture of the Membranes
Premature rupture of the membranes, or PROM, occurs when the amniotic sac ruptures before labor. That means the mother’s “water broke” before she was in full active labor. This is a medical emergency and the mother should get medical attention immediately. The amniotic sac and fluid is what protects the baby. Without adequate protection, the baby is at risk for birth injuries like hypoxic ischemic encephalopathy (HIE), brain damage, cerebral palsy, meningitis, sepsis, and more.
Primiparous Mother (first birth)
In pregnancies where it is the mother’s first time giving birth, complications like caput succedaneum are more likely. That’s because the mother’s body has not been through the labor and delivery process before.
Oligohydramnios
Amniotic fluid is the fluid inside the amniotic sac. It is primarily made from water, but as the fetus grows and begins to urinate, the amniotic fluid becomes a mixture of water and urine. As the fetus grows, so does the volume of amniotic fluid. Amniotic fluid is important for growth and nutrition, protection from movements or trauma, and helps the baby maintain their body temperature.
When there is not enough amniotic fluid in the sac to protect the baby, the mother may be diagnosed with oligohydramnios. A lack of amniotic fluid can be caused by:
- Placental insufficiency
- Birth defects
- Preeclampsia
- Post-term pregnancy
When the mother has oligohydramnios, it means that the baby is at risk for a birth injury, such as:
- Intrauterine growth restriction
- Premature birth
- Meconium aspiration syndrome
- HIE
- Cerebral Palsy
- Death
Birth Assisting Tools
Using a vacuum extraction tool or forceps during delivery also increases the risk of caput succedaneum, primarily because the vacuum must draw the soft tissue up into the vacuum cup to be able to control the delivery. This is particularly a concern in babies with macrosomia, or those that are proportionally too large for the birth canal and mother’s pelvic bones. Improper use of forceps or a vacuum is a leading cause of birth injuries.
Can Medical Negligence Cause Caput Succedaneum?
While conditions like macrosomia or oligohydramnios occur due to natural medical factors, it is important that doctors recognize risk factors and signs of complications, and that they act immediately to prevent a birth injury. There are situations where caput succedaneum may be caused by medical negligence, such as if the doctor knows the baby is too large for a vaginal delivery but does not order a c-section instead. Furthermore, if medical professionals improperly use forceps or a vacuum extractor and cause injuries to the baby, they can be held liable for their actions. Speak with a birth injury lawyer to learn more.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.
Symptoms of Caput Succedaneum
If your baby has caput succedaneum, the most obvious symptom is the conehead like appearance of the infant’s head.

There are other symptoms that you should be aware of, however, such as:
- Puffiness under the skin of the scalp (the most prominent symptom)
- Bruising and/or color changes to the scalp
- Molding increase on the head
- Scalp swelling across the infant’s midline and suture lines
No formal testing is usually needed or performed to diagnose caput succedaneum. Instead, a physician will perform a physical examination and assess the symptoms to make a formal diagnosis.
It is important to remember that the symptoms of caput succedaneum are similar to that of other conditions like cephalohematoma or hydrocephalus. These are both serious medical conditions that require immediate medical care. Caput succedaneum, on the other hand, is not a medical emergency. Your doctor should be able to differentiate between similar conditions and make an accurate diagnosis.
Difference Between Caput Succedaneum and Cephalohematoma
While similar, there are differences between caput succedaneum and cephalohematoma. Unlike caput succedaneum, which is a minor birth injury from fluid buildup, cephalohematoma is a hemorrhage of blood that pools under the scalp. With cephalohematoma, tiny blood vessels rupture due to pressure during delivery, which causes blood to pool up in that area. Generally, cephalohematomas resolve on their own in a few weeks, up to a few months. However, infections or abscesses can form, especially if doctors attempt to drain the blood. There is also a risk that the baby could be anemic due to blood loss, in which cases a blood transfusion may be necessary.
Treating Caput Succedaneum
Caput succedaneum is certainly alarming to new parents. The good news is that the condition often resolves itself within a few days. No treatment is usually necessary. In fact, attempting to drain the scalp area may lead to infections that will only make things worse. However, since the bruising caused by caput succedaneum may break down into bilirubin, there is a heightened risk of the baby developing jaundice. Jaundice occurs when there is excess bilirubin in the blood. Most parents recognize it by the yellowing of the baby’s skin or eyes.
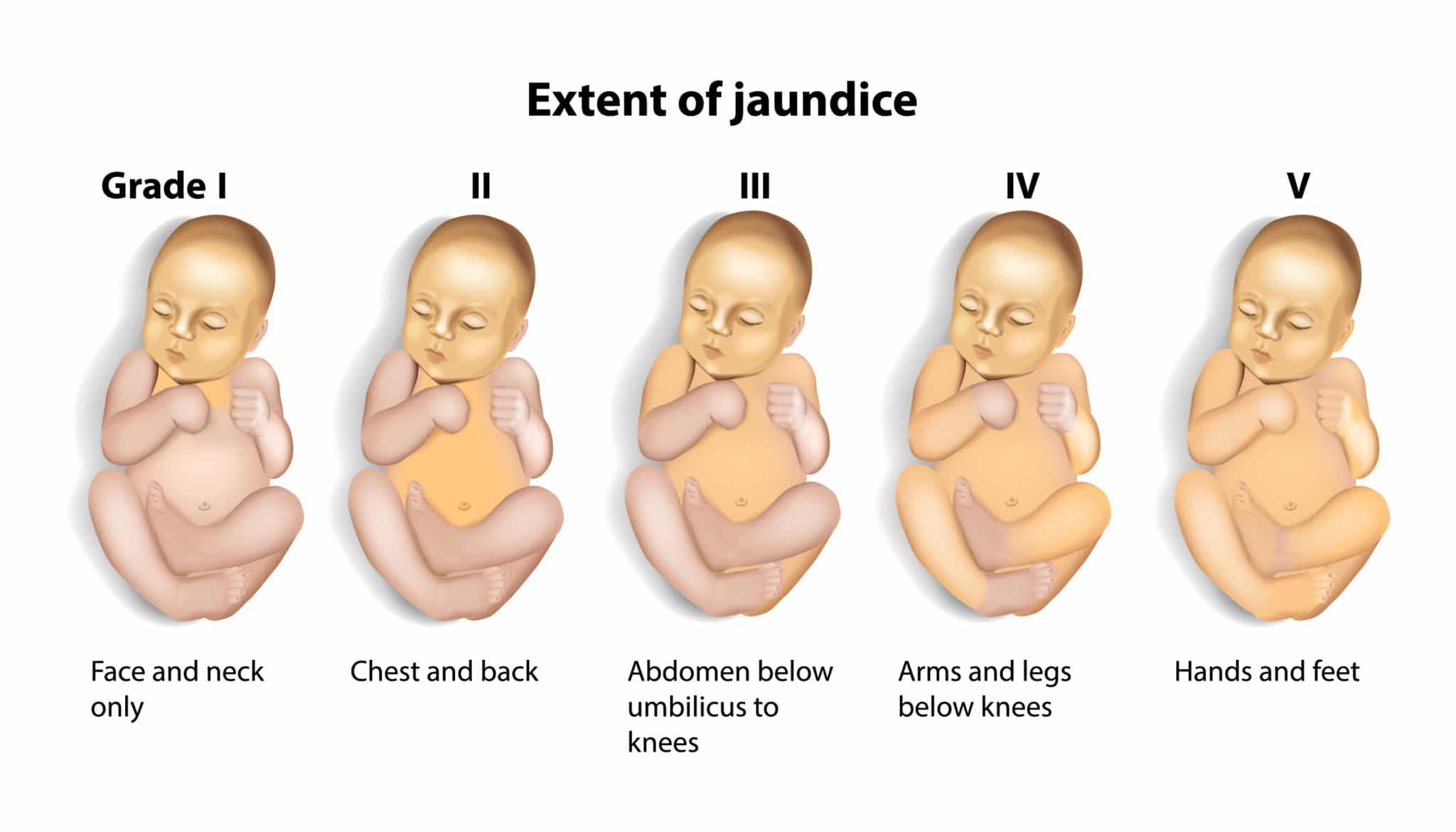
Jaundice, if treated properly and quickly, typically is not a serious medical issue. However, if left undiagnosed and untreated, jaundice may lead to severe medical issues, including brain damage (kernicterus) and in severe cases, death. If your baby develops jaundice, they will be treated using phototherapy. This treatment requires the baby to be placed under special lights or under a lighted blanket. The light helps the baby’s body break down bilirubin and excrete it. Generally, this treatment is effective at treating jaundice without any complications. Sometimes, however, if jaundice is not diagnosed immediately, or if it is severe, the baby can suffer brain damage due to bilirubin entering brain tissue (see kernicterus).
Prognosis for Caput Succedaneum
In most cases, the prognosis for caput succedaneum is good. If there is minimal or no bruising and no signs of jaundice or infection, the baby will likely have no long-term medical issues. However, if the baby develops complications like jaundice, the prognosis may change due to the impact of those medical conditions. For example, if the baby develops jaundice that’s treated immediately, there are usually no long-term problems associated with caput succedaneum. As the baby’s scalp begins to heal within a few days, the head will return to its normal size and shape. However, as previously mentioned, untreated jaundice can lead to several long-term complications, including Kernicterus, a form of brain damage.
Kernicterus or brain damage can cause long-term or lifelong medical conditions that can definitely affect your child’s prognosis. Some of the possible outcomes of brain damage are:
- Athetoid cerebral palsy
- Hearing loss
- Poor tooth enamel development
- Permanent upward gaze
Conditions like cerebral palsy are lifelong disorders that will certainly affect your child’s treatment and overall medical care. Any birth injury can be devastating for your family, but it’s important to know that you aren’t alone.
How to Optimize Your Child’s Prognosis
Many parents are often scared and confused at the appearance of an infant with caput succedaneum. The best way to improve your child’s prognosis is to be involved in their care every step of the way. If you notice it looks like the bruising is getting worse or there is new swelling, talk to your baby’s doctor. Also, be aware of the symptoms of conditions like jaundice, which can cause complications if not treated right away. You know your baby better than anyone, so look out for signs that something isn’t quite right and take action.
If your child does develop jaundice or has a more serious birth injury like kernicterus, be active in their care and treatment plan. Don’t underestimate how seemingly harmless a condition like jaundice is. Make sure your baby gets the care that they need.



